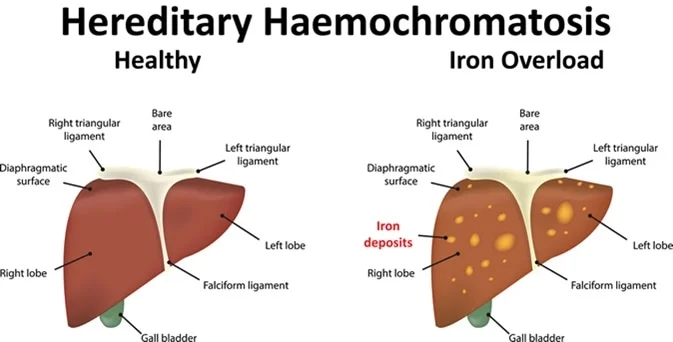
Hereditary hemochromatosis (he-moe-kroe-muh-TOE-sis) causes your body to absorb too much iron from the food you eat. Excess iron is stored in your organs, especially your liver, heart and pancreas. Too much iron can lead to life-threatening conditions, such as liver disease, heart problems and diabetes.
The genes that cause hemochromatosis are inherited, but only a minority of people who have the genes ever develop serious problems. Signs and symptoms of hereditary hemochromatosis usually appear in midlife.
Treatment includes regularly removing blood from your body. Because much of the body’s iron is contained in red blood cells, this treatment lowers iron levels.
Symptoms
Some people with hereditary hemochromatosis never have symptoms. Early signs and symptoms often overlap with those of other common conditions.
Signs and symptoms may include:
- Joint pain
- Abdominal pain
- Fatigue
- Weakness
- Diabetes
- Loss of sex drive
- Impotence
- Heart failure
- Liver failure
- Bronze or gray skin color
- Memory fog
Causes
Hereditary hemochromatosis is caused by a mutation in a gene that controls the amount of iron your body absorbs from the food you eat. These mutations are passed from parents to children. This type of hemochromatosis is by far the most common type.
Gene mutations that cause hemochromatosis
A gene called HFE is most often the cause of hereditary hemochromatosis. You inherit one HFE gene from each of your parents. The HFE gene has two common mutations, C282Y and H63D. Genetic testing can reveal whether you have these mutations in your HFE gene.
- If you inherit 2 abnormal genes, you may develop hemochromatosis. You can also pass the mutation on to your children. But not everyone who inherits two genes develops problems linked to the iron overload of hemochromatosis.
- If you inherit 1 abnormal gene, you’re unlikely to develop hemochromatosis. However, you are considered a gene mutation carrier and can pass the mutation on to your children. But your children wouldn’t develop the disease unless they also inherited another abnormal gene from the other parent.
How hemochromatosis affects your organs
Iron plays an essential role in several body functions, including helping in the formation of blood. But too much iron is toxic.
A hormone called hepcidin, secreted by the liver, normally controls how iron is used and absorbed in the body, as well as how excess iron is stored in various organs. In hemochromatosis, the normal role of hepcidin is disrupted, causing your body to absorb more iron than it needs.
This excess iron is stored in major organs, especially your liver. Over a period of years, the stored iron can cause severe damage that may lead to organ failure and chronic diseases, such as cirrhosis, diabetes and heart failure. Though many people have faulty genes that cause hemochromatosis, not everyone develops iron overload to a degree that causes tissue and organ damage.
Hereditary hemochromatosis isn’t the only type of hemochromatosis. Other types include:
- Juvenile hemochromatosis. This causes the same problems in young people that hereditary hemochromatosis causes in adults. But iron accumulation begins much earlier, and symptoms usually appear between the ages of 15 and 30. This disorder is caused by mutations in the hemojuvelin or hepcidin genes.
- Neonatal hemochromatosis. In this severe disorder, iron builds up rapidly in the liver of the developing baby in the womb. It is thought to be an autoimmune disease, in which the body attacks itself.
- Secondary hemochromatosis. This form of the disease is not inherited and is often referred to as iron overload. People with certain types of anemia or chronic liver disease may need multiple blood transfusions, which can lead to excess iron accumulation.
Risk factors
Factors that increase your risk of hereditary hemochromatosis include:
- Having 2 copies of a mutated HFE gene. This is the greatest risk factor for hereditary hemochromatosis.
- Family history. If you have a first-degree relative — a parent or sibling — with hemochromatosis, you’re more likely to develop the disease.
- Ethnicity. People of Northern European descent are more prone to hereditary hemochromatosis than are people of other ethnic backgrounds. Hemochromatosis is less common in people of Black, Hispanic and Asian ancestry.
- Your sex. Men are more likely than women to develop signs and symptoms of hemochromatosis at an earlier age. Because women lose iron through menstruation and pregnancy, they tend to store less of the mineral than men do. After menopause or a hysterectomy, the risk for women increases.
Complications
Untreated, hereditary hemochromatosis can lead to a number of complications, especially in your joints and in organs where excess iron tends to be stored — your liver, pancreas and heart. Complications can include:
- Liver problems. Cirrhosis — permanent scarring of the liver — is just one of the problems that may occur. Cirrhosis increases your risk of liver cancer and other life-threatening complications.
- Diabetes. Damage to the pancreas can lead to diabetes.
- Heart problems. Excess iron in your heart affects the heart’s ability to circulate enough blood for your body’s needs. This is called congestive heart failure. Hemochromatosis can also cause abnormal heart rhythms (arrhythmias).
- Reproductive problems. Excess iron can lead to erectile dysfunction (impotence), and loss of sex drive in men and absence of the menstrual cycle in women.
- Skin color changes. Deposits of iron in skin cells can make your skin appear bronze or gray in color.
The list of some Hemochromatosis medicine: