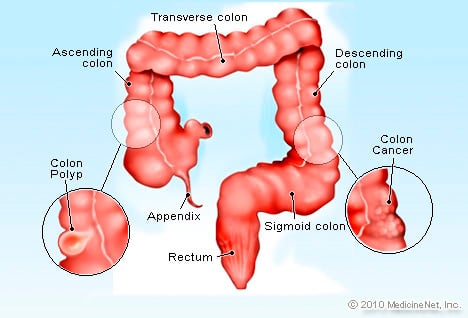
The large intestine is the last part of the digestive tract. It has two components: the colon, which makes up the first six feet of the large intestine, and the rectum, which makes up the last six inches and ends in the anus. Cancers of the colon and rectum are often grouped together as colorectal cancer.
Colorectal cancers occur when the cells of the colon or rectum divide uncontrollably. The majority of colorectal cancers start as polyps, which are small overgrowths of tissue in the lining of the colon. Most polyps are benign (non-cancerous), but some may grow out of control and become cancerous.
More specifically, most cases of colorectal cancer are adenocarcinomas. Adenocarcinoma refers to cancers that begin in the mucus-producing gland cells that line the intestine. These gland cells can be found within polyps. While there are a few other types of colon cancers, they are rare and treated differently.
Most precancerous polyps produce few if any symptoms, so it is important to get screened regularly for colon cancer. Colorectal cancer screenings allow your doctor to find ad remove polyps before they turn into cancer.
To learn more about colon cancer screenings, visit our Colorectal Cancer Screening Exams page.
Types of Colon cancer
The majority of colorectal cancers are adenocarcinomas that began as adenomas, which are a type of polyp that may become cancer.
Symptoms
- Colorectal cancer usually starts off in small polyps (overgrowth of tissue) in the colon or rectum. These polyps may not produce any symptoms, especially in the early stages. As the disease progresses, more symptoms may appear.
- Symptoms of colorectal cancer may include:
- Diarrhea or constipation that does not go away
- Change in normal bowel habits, such as size, shape, and frequency
- Discomfort or urge to have a bowel movement when there is no need
- Abdominal pain or cramping pain in your lower stomach
- Bloating or full feeling
- Change in appetite
- Rectal bleeding
- Blood in the stool or toilet after a bowel movement
- Excessive fatigue
- Weight loss without dieting
- In the later stages of colon cancer, the polyp may metastasize (spread) to other parts of the body. This can cause other symptoms, depending on where cancer has spread.
- These symptoms usually do not mean you have colorectal cancer. But, any time you notice unexplained changes and they persist for more than two weeks, don’t assume they will just go away. See your doctor.
Risk factors
Anything that increases your chance of getting colorectal cancer is a risk factor. Colorectal cancer risk factors include:
- Age: Colorectal cancer is most frequently diagnosed in people aged 65-74.
- Race: African Americans have the highest rate of colon cancer among all racial groups in the United States.
- Family history of colon cancer, rectal cancer, or polyps
- Inflammatory bowel disease (Crohn’s disease or chronic ulcerative colitis)
- Prior history of colorectal cancer or polyps
- Hereditary cancer syndromes: Some genetic mutations can be inherited and increase your risk for certain types of cancer. Inherited syndromes including hereditary nonpolyposis colorectal cancer (HNPCC or Lynch syndrome and familial adenomatous polyposis (FAP) may put you at higher risk for developing colon cancer.
For patients concerned about inherited family syndromes that cause colorectal cancer, we offer advanced genetic testing and counseling to help understand your risk.
Lifestyle factors that increase your colorectal cancer risk include:
- Obesity
- Lack of exercise
- Diet: If you eat a lot of red meat, processed meats, or meats cooked at very high heat, you may be at higher risk for colon cancer
- Sedentary lifestyle
- Cigarette smoking
- Drinking too much alcohol
Treatment
Screening for colorectal cancer
Doctors recommend certain screening tests for healthy people with no signs or symptoms in order to look for signs of colon cancer or noncancerous colon polyps. Finding colon cancer at its earliest stage provides the greatest chance for a cure. Screening has been shown to reduce your risk of dying of colon cancer.
Doctors generally recommend that people with an average risk of colon cancer begin screening around age 50. But people with an increased risk, such as those with a family history of colon cancer or African-American heritage, should consider screening sooner.
Several screening options exist — each with its own benefits and drawbacks. Talk about your options with your doctor, and together you can decide which tests are appropriate for you. If a colonoscopy is used for screening, polyps can be removed during the procedure before they turn into cancer.
Diagnosing colon cancer
If your signs and symptoms indicate that you could have colon cancer, your doctor may recommend one or more tests and procedures, including:
- Using a scope to examine the inside of your colon (colonoscopy). Colonoscopy uses a long, flexible and slender tube attached to a video camera and monitor to view your entire colon and rectum. If any suspicious areas are found, your doctor can pass surgical tools through the tube to take tissue samples (biopsies) for analysis and remove polyps.
- Blood tests. No blood test can tell you if you have colon cancer. But your doctor may test your blood for clues about your overall health, such as kidney and liver function tests.
Your doctor may also test your blood for a chemical sometimes produced by colon cancers (carcinoembryonic antigen, or CEA). Tracked over time, the level of CEA in your blood may help your doctor understand your prognosis and whether your cancer is responding to treatment.
Determining the extent of the cancer
If you’ve been diagnosed with colon cancer, your doctor may recommend tests to determine the extent (stage) of your cancer. Staging helps determine what treatments are most appropriate for you.
Staging tests may include imaging procedures such as abdominal, pelvic and chest CT scans. In many cases, the stage of your cancer may not be fully determined until after colon cancer surgery.
The stages of colon cancer are indicated by Roman numerals that range from 0 to IV, with the lowest stages indicating cancer that is limited to the lining of the inside of the colon. By stage IV, the cancer is considered advanced and has spread (metastasized) to other areas of the body.
The list of some Colorectal medicine: