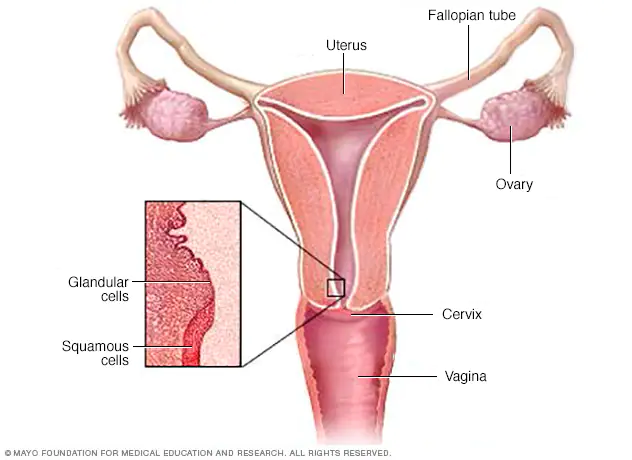
Cervical cancer starts in the cells lining the cervix — the bottom part of the uterus (womb). The cervix connects the body of the uterus (the upper part where a fetus grows) to the fanny (birth canal). Cancer begins when cells in the body begin to increase of control.
The cervix is made of two parts and is covered with two different types of cells.
• The endocervix is the opening of the cervix that leads into the uterus. It is covered with glandular cells.
• The exocervix (or ectocervix) is the outer part of the cervix that can be seen by the doctor during a speculum exam. It is covered in squamous cells.
The place where these two cell types meet in the cervix is called the transformation zone. The exact location of the transformation zone changes as you get older and if you give birth. Most cervical cancers begin in the cells in the transformation zone.
Types of cervical cancer
Cervical cancers and cervical pre-cancers are classified by how they look in the labs with a microscope. The main types of cervical cancers are squamous cell carcinoma and adenocarcinoma.
- Most (up to 9 out of 10) cervical cancers are squamous cell carcinomas. These cancers develop from cells in the exocervix. Squamous cell carcinomas most often begin in the transformation zone (where the exocervix joins the endocervix).
- Most of the other cervical cancers are adenocarcinomas. Adenocarcinomas are cancers that develop from glandular cells. Cervical adenocarcinoma develops from the mucus-producing gland cells of the endocervix.
- Less commonly, cervical cancers have features of both squamous cell carcinomas and adenocarcinomas. These are called adenosquamous carcinomas or mixed carcinomas.
Although almost all cervical cancers are either squamous cell carcinomas or adenocarcinomas, other types of cancer also can develop in the cervix. These other types, such as melanoma, sarcoma, and lymphoma, occur more commonly in other parts of the body.
Cancer is the result of the uncontrolled division and growth of abnormal cells. Most of the cells in our body have a set lifespan, and, when they die, the body generates new cells to replace them.
Abnormal cells can have two problems:
- they do not die
- they continue dividing
This results in an excessive buildup of cells, which eventually forms a lump or tumor. Scientists are not completely sure why cells become cancerous.
However, some risk factors might increase the risk of developing cervical cancer. These include:
- HPV: This is a sexually transmitted virus. More than 100 different types of HPV can occur, at least 13 of which may cause cervical cancer.
- Having many sexual partners or becoming sexually active early: The transmission of cancer-causing HPV types nearly always occurs as a result of sexual contact with an individual who has HPV. Women who have had many sexual partners generally have a higher risk of HPV infection. This increases their risk of developing cervical cancer.
- Smoking: This increases the risk of cervical cancer, as well as other types.
- A weakened immune system: The risk of cervical cancer is higher in those with HIV or AIDS, and people who have undergone a transplant, leading to the use of immunosuppressive medications.
- Birth control pills: Long-term use of some common contraceptive pills slightly raises a woman’s risk.
- Other sexually transmitted diseases (STD): Chlamydia, gonorrhea, and syphilis increase the risk of developing cervical cancer.
- Socio-economic status: Rates appear to be higher in areas where income is low.
Cervical cancer treatment options include surgery, radiotherapy, chemotherapy, or combinations of these.
Deciding on the kind of treatment depends on several factors, such as the stage of cancer, as well as age and overall state of health.
Treatment for early-stage cervical cancer, when cancer remains within the cervix, has a good success rate. Further cancer spreads from its original area, the lower the success rate tends to be.
Early-stage options
Surgery is a common treatment method when the cancer has not spread from the cervix. Radiation therapy may help after surgery if a doctor believes that cancer cells might be present inside the body.
Radiation therapy may also reduce the risk of recurrence (cancer coming back). If the surgeon wants to shrink the tumor to make it easier to operate, the person may receive chemotherapy although this is not a very common approach.
Treatment for advanced cervical cancer
When the cancer has spread beyond the cervix, surgery is not usually an option.
Doctors also refer to advanced cancer as invasive cancer, because it has invaded other areas of the body. This type of cancer requires more extensive treatment, which will typically involve either radiation therapy or a combination of radiation therapy and chemotherapy.
In the later stages of cancer, healthcare professionals provide palliative therapy to relieve symptoms and improve quality of life.
Doctors from different specialties frequently work together to treat breast cancer. Surgeons are doctors who perform operations. Medical oncologists are doctors who handle cancer with drugs. Radiation oncologists are doctors who treat cancer with radiation.
The list of some Cervical Cancer medicine: